Antimicrobial resistance (AMR) is becoming one of the biggest health and societal threats today. Recognising the severity of this problem, clinical microbiology company Quantamatrix has developed innovative technologies to help tackle the issue.
The issue of antimicrobial resistance poses a threat not only to individual health but also to the safety of society as a whole. Resistant bacteria can spread between individuals, crossing borders and proliferating globally, potentially leading to large-scale outbreaks akin to a ‘pandemic’, which places a tremendous burden on public health systems.
The World Health Organization (WHO) refers to AMR as a ‘silent pandemic’ and has classified it as one of the top ten threats to global public health. According to the international medical journal The Lancet, more than one million people have died each year from drug-resistant infections as a direct cause of death between 1990 and 2021, with projections suggesting that this number could reach two million annually by 2050. Additionally, the UK’s antimicrobial resistance report by Jim O’Neill warns that, if AMR is not adequately addressed, the number of direct and indirect deaths from AMR could exceed ten million worldwide by 2050, surpassing the eight million deaths caused by cancer.
Reasons for AMR and the global issue of AMR: The One Health Initiative
The primary cause of AMR is the misuse and overuse of antimicrobials. For instance, during the pandemic, antimicrobials, antifungals, and AR antimicrobials were indiscriminately used on COVID-19 patients, despite their ineffectiveness against the virus, exacerbating the AMR problem. Additionally, as medical facilities, resources, and personnel were concentrated on responding to COVID-19, infection prevention, surveillance, control, and appropriate treatment for potential AMR patients weakened, leading to an increase in antimicrobial-resistant bacteria.
Particularly concerning is the continuous rise of antimicrobial-resistant pathogens known as ‘superbugs’, which are no longer responsive to antimicrobials, viruses, fungi, and parasites, further deepening the AMR crisis.
To address this AMR issue, the global initiative known as ‘One Health’ has been launched. One Health aims to tackle the worldwide AMR problem through a four-part collaboration involving the World Health Organization (WHO), the Food and Agriculture Organization (FAO), the World Organisation for Animal Health (WOAH), and the United Nations Environment Programme (UNEP). In a new declaration made during the UN high-level meeting on AMR in September, it was pledged to reduce deaths caused by AMR by 10% over the next six years, in response to the ‘silent slow-motion pandemic’ that could claim around 39 million lives by 2050.
Moreover, the initiative recognises the close interconnection between human health, animal health, and the environment, emphasising the need to strengthen strategic co-operation at local, national, and global levels regarding not only human and animal health but also food security, environmental issues, and economic concerns.
Antimicrobial resistance issues in Europe
In the European Union (EU) and the European Economic Area (EEA), the costs associated with antimicrobial resistance were estimated to reach approximately €1.5bn annually as of 2022. In 2022 alone, over 35,000 people died from drug-resistant bacterial infections in Europe. This figure surpasses the combined death toll from influenza, tuberculosis, and HIV/AIDS, indicating that if the spread of resistant bacteria continues, it could have severe repercussions not only on public health systems but also across society as a whole.
However, the EU lags behind the United States, China, the United Kingdom, India, and Australia in the field of AMR research. Even Germany, which has published the most papers in the EU, has only around 6,000 publications, which is half the number of those from the UK or India. Furthermore, none of the top ten institutions in antimicrobial resistance research are located within the EU, suggesting a relatively low concentration of AMR research in the region.
Importance of rapid diagnostics in overcoming AMR
In the medical field directly addressing the AMR issue, close collaboration among healthcare professionals, industry, and government is essential to overcome this challenge. Stabilising the supply chain for existing antimicrobials, developing new antimicrobials, and implementing ‘rapid diagnostics’ to prevent the misuse of antimicrobials are all crucial.
Particularly when bacterial bloodstream infections progress to sepsis, the survival rate declines sharply by 7-9% per hour after onset, leading to a 30% mortality rate within 30 days. Current diagnostic methods often involve the empirical use of broad-spectrum antimicrobials, which can take a long time to identify the optimal antimicrobial treatment, thereby accelerating the problem of antimicrobial resistance and threatening patient lives.
Therefore, rapid and accurate diagnostics are vital, as timely treatment with the correct antimicrobials can significantly impact patient outcomes. Recognising this need early on, the innovative company in clinical microbiology, Quantamatrix, has developed dRAST™ and uRAST to achieve faster and more accurate diagnostics.
Quantamatrix and dRAST™
Quantamatrix was established in 2010 as a spin-off from the laboratory of Professor Kwon Sung-hoon in the Department of Electrical Engineering at Seoul National University, South Korea. CEO Kwon founded the company with the goal of developing innovative platforms in clinical microbiology and molecular/immunodiagnostics to save patients’ lives through early diagnosis and improve healthcare environments.
In 2016, Quantamatrix developed the dRAST solution (direct & Rapid Antimicrobial Susceptibility Testing), which revolutionised the field of clinical microbiological diagnostics. While traditional antimicrobial susceptibility testing (AST) typically takes about 60 hours, dRAST significantly reduces this testing time by 30 to 50 hours, allowing for quicker and more effective treatment decisions.
Three core proprietary technologies of dRAST
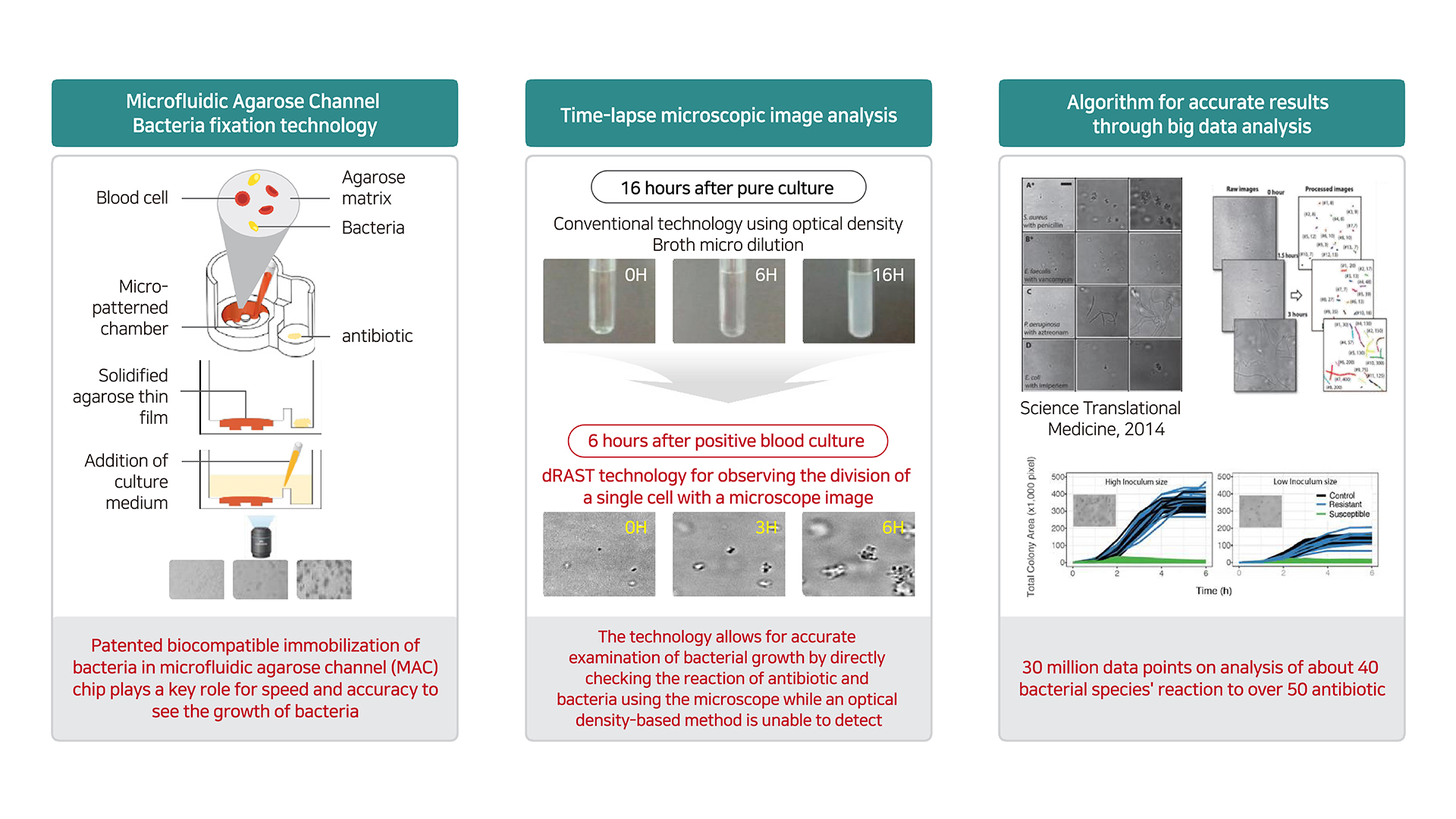
The rapid diagnostic capability of dRAST is attributed to three core proprietary technologies:
- Microfluidics and bacterial immobilisation technology: This technology allows for the effective mixing of positive blood culture samples with agarose, which is then dispensed onto a chip and gelled to immobilise the bacteria within a thin layer of agarose.
- Microscopic imaging: dRAST employs advanced microscopic imaging techniques to capture time-series images of bacterial growth. This allows for real-time monitoring of bacterial activity.
- AI-driven big data analysis: Using algorithms trained through artificial intelligence (AI), dRAST can quickly assess bacterial growth or non-growth based on the imaging data. Traditional antimicrobial susceptibility testing (AST) methods, used globally for over 30 years, primarily relied on turbidity changes due to metabolic activity when bacteria encounter antimicrobials, which required waiting for physical metabolic processes and thus took a long time. In contrast, dRAST conducts AST directly from positive blood cultures, determining the effectiveness of antimicrobials within five to seven hours.
dRAST is optimised for testing both Gram-positive and Gram-negative bacteria, offering advantages in daily testing capacity, antimicrobial diversity, concentration composition for each antimicrobial, ease of use, and convenient reagent storage, making it a comprehensive rapid diagnostic solution.
dRAST’s global market penetration
dRAST was commercialised for the first time in the world at Seoul National University Hospital in South Korea in 2019. Following this, the same year, Quantamatrix established its European subsidiary in Paris, France, to directly target the global market. They have secured over 50 customer hospitals in key countries, including Germany, the UK, France, and Switzerland, as well as in Spain, Portugal, Poland, the Czech Republic, and Romania, accelerating their commercialisation efforts.
Recently, Quantamatrix has also expanded into the Middle East, entering markets in Saudi Arabia, Kuwait, Oman and the UAE, as well as Southeast Asia, further promoting market growth.
Clinical trial results of dRAST: Ramon Y Cajal
In April, at the largest European clinical microbiology and infectious diseases conference, ‘ESCMID Global 2024,’ results were presented from a study conducted over the past year at a hospital in Spain involving 300 patients, focusing on the ‘clinical and economic utility of dRAST’. The rapid test results provided by dRAST enabled prompt prescription of appropriate antimicrobials, reducing the 30-day mortality rate for severe sepsis patients from 24.4% to 9.5%, a decrease of 14.9 percentage points. For all patients with bacteremia, the 30-day mortality rate dropped from 13.5% to 9.6% with dRAST use, representing a reduction of 3.9 percentage points. This suggests that, for every 26 dRAST tests performed, one patient’s life can be saved.
Additionally, in the economic evaluation of hospital operations, a frequently used metric is the average length of stay in the intensive care unit (ICU), which decreased from 12.4 days to six days, a reduction of over six days. Quantifying this change indicates a potential direct healthcare cost savings of approximately €13,440. Reducing patient length of stay increases bed turnover, allowing hospitals to accommodate more new patients, thereby enhancing operational efficiency and expanding economic benefits. The use of dRAST not only saves lives but also demonstrates significant economic and social value.
Next-generation technology, uRAST
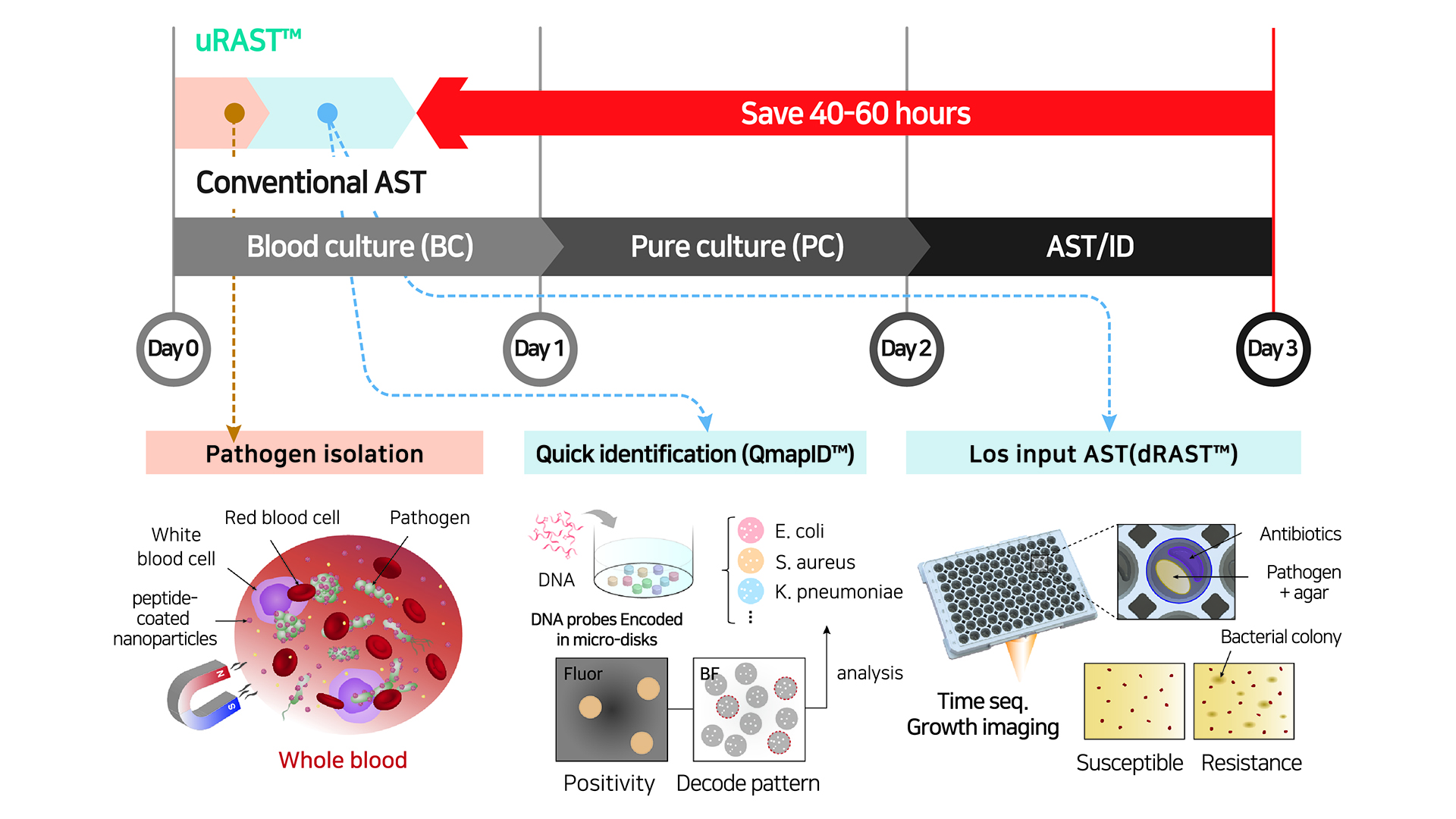
In July, Quantamatrix developed the all-in-one rapid antimicrobial susceptibility testing technology, uRAST (ultra-Rapid Antimicrobial Susceptibility Testing), which integrates all processes before AST, completing all tests in just 13 hours. This technology was developed in collaboration with Seoul National University and Seoul National University Hospital and was introduced in July in the prestigious journal Nature (Impact factor: 64.8 in 2022).1
The ‘uRAST’ technology combines Quantamatrix’s ‘dRAST’ technology with the bacterial identification technology ‘QmapID (QuantaMatrix Multi Assay Platform IDentification),’ allowing the entire process to be completed in one day. Notably, the QmapID technology utilises a method of inscribing specific codes onto microdisks smaller than a hair cross-section, enabling the specific differentiation of 50 to 100 different bacterial species in a single test. This innovation significantly reduces the physical workload and time required for bacterial identification. Together with dRAST, the uRAST technology is regarded as an innovative solution to address the issue of AMR.
Future aspirations
Kwon Sung-hoon, CEO, stated: “After commercialising dRAST, I set a goal to innovate by integrating reverse processes such as bacterial identification and blood culture. The biggest challenge was whether we could eliminate the time-consuming blood culture process. Through dedicated research to solve this issue, we were able to develop the uRAST technology, which led to our achievements being featured in Nature.
“We aim to bring about another disruptive change with μCIA (micro Culture-Identification-AST), an integrated testing solution that commercialises the uRAST technology in the rapid AST market led by our current flagship product, dRAST. While continuously pursuing the global expansion of dRAST, we are committed to developing the all-in-one testing system μCIA to showcase yet another innovation in the field of clinical microbiology diagnostics.”
References
Please note, this article will also appear in the 20th edition of our quarterly publication.
This post was originally published on here







