Scientists at City of Hope, one of the leading cancer research and treatment centres in the U.S., have identified a key protein that helps cancer cells avoid detection by the immune system during a type of advanced therapy. The identification of the YTHDF2 protein is a significant breakthrough in cancer treatment. This CAR T cell therapy is effective against blood cancers like leukaemia and lymphoma, but many cancer cells have developed mechanisms to hide from it.
By creating a new drug that blocks this protein, researchers hope to make cancer treatments more effective, especially for hard-to-treat blood cancers. This breakthrough could lead to better survival rates and fewer relapses for patients.
What is CAR T cell therapy?
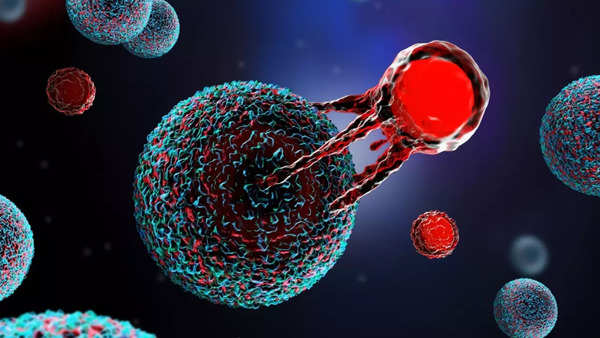
Chimeric antigen receptor (CAR) T-cell therapy is a cancer treatment that genetically alters a patient’s T cells to help them recognize and destroy cancer cells. The advanced CAR T cell therapy is a cancer treatment that trains the immune system to find and destroy tumour cells. It is commonly used for certain types of leukaemia and lymphoma, both of which are blood cancers.
However, some cancer cells have developed ways to hide from the immune system, making the treatment less effective. A new study published today (December 17) in the journal Cell could pave the way for more personalized therapies that improve patient outcomes.
Researchers identified a protein called YTHDF2, which plays a critical role in helping blood cancer cells survive and spread. In response, City of Hope developed a new drug compound called CCI-38. This compound targets and suppresses YTHDF2, slowing the growth of aggressive blood cancers and increasing the chances of successful treatment.
What the research says….
Jianjun Chen, Ph.D., Simms/Mann Family Foundation Chair in Systems Biology and the director of the Centre for RNA Biology and Therapeutics at Beckman Research Institute of City of Hope, and corresponding author of the new study, said, “We believe that using CCI-38 to target YTHDF2 will significantly enhance the effectiveness of CAR T cell therapy on blood cancer cells. One of the challenges in treating blood cancers is a phenomenon called ‘antigen escape.’ A key target for these therapies is a protein called CD19 found on the cancer cells.”
However, in 28-68% of cases, the cancer cells lower or lose this CD19 marker, making treatments less effective. Although researchers are working on strategies to target multiple components, nearly half of patients are still affected by this issue.
YTHDF2 switches on genes that help cancer cells produce a stable energy source to fuel the cells’ ability to grow and spread. Moreover, this protein helps cancer cells conceal themselves by reducing the presence of antigen biomarkers that normally trigger the immune system to detect and attack cancer.
The way forward:
The research team has developed a new drug, CCI-38, that targets and suppresses YTHDF2, potentially enhancing the effectiveness of CAR T cell therapy. This could lead to improved survival rates and fewer relapses for patients. YTHDF2 not only aids cancer cell survival but also reduces key antigen markers that the immune system uses to detect tumours.
The findings, published in Cell, suggest that targeting this protein may offer personalized treatment options for patients who do not respond to current therapies. City of Hope is now focusing on further improving CCI-38’s safety and effectiveness, with plans for clinical trials ahead.
Zhen-Hua Chen, Ph.D., a staff scientist in systems biology at Beckman Research Institute of City of Hope and first author of the study, said, “Unravelling the biology underlying YTHDF2’s function will help us develop new strategies to prevent tumour cells from escaping immune surveillance. This could lead to personalized approaches for patients whose blood cancers don’t respond to initial treatment or who relapse after initial response to T cell-based immunotherapy.”
Xiaolan Deng, Ph.D., an associate research professor in systems biology at Beckman Research Institute of City of Hope and a co-corresponding author of the study, said, “Reducing the need for follow-up treatments could lead to better long-term survival and less relapse for our patients while lowering side effects and medical costs.”
This post was originally published on here







