This post was originally published on here
Eradicating cervical cancer may require vaccinating against the human papillomavirus not just in girls but in boys as well, a new study suggests.
The virus, commonly known as HPV, is responsible for the most widespread sexually transmitted infection in the world but current vaccination drives only target girls.
Although the infection can remain without any symptoms and resolve naturally within two years in 90 per cent of the cases, its persistence can lead to cancer in some people.
HPV-induced cervical cancer is the fourth most common cancer in women, with nearly 660,000 new cases and 350,000 deaths every year.
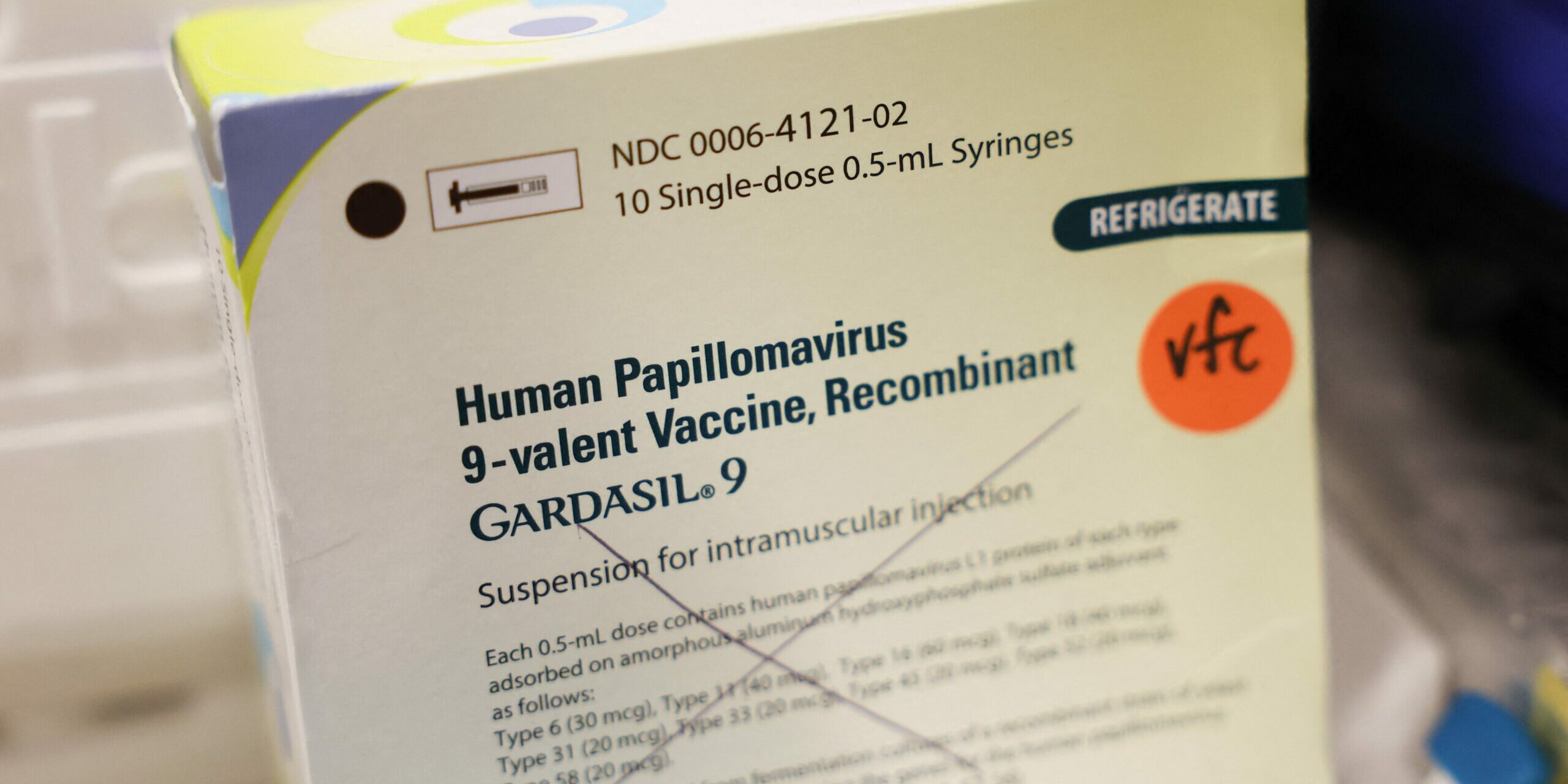
HPV vaccines, shown to be effective in minimising disease spread and cancer risk, are currently offered and recommended in 147 countries.
But the best vaccination strategy to eradicate HPV-induced cervical cancer remains debatable, researchers say.
Now scientists have come up with a new mathematical model to help public health officials design more effective HPV vaccination programmes.
The model, detailed in a new study published in the journal Bulletin of Mathematical Biology, assessed whether a recent HPV vaccination programme in South Korea was enough to control cervical cancer.
Researchers found that vaccinating boys against HPV, along with ongoing efforts to immunise girls, could be key to eradicating cervical cancer.
“Cervical cancer is one of the few cancers effectively prevented by vaccines,” Soyoung Park, lead author of the study from the University of Maryland, said. “It was important to check if the recent government program for offering vaccines is going to be enough to effectively control the disease in Korea.”
The new model incorporates demographic and South Korean cervical cancer data from 1999 to 2020 to predict how HPV transmits across a population.
South Korea’s National Immunisation Programme, which started in 2016, vaccinates about 80 per cent of the nation’s girls aged 12-17 while another 30,000 women aged 18-26 receive “catch-up vaccinations” annually.
The model shows these policies are insufficient to eliminate HPV and related cancers in the country.
“It’s achieving the objective of reducing cases of cervical cancer, but it’s not going to eliminate it. The objective is elimination,” Abba Gumel, another study author, said.
To completely eradicate cervical cancer, researchers estimate that the immunisation drive must cover 99 per cent of women in the country. But vaccinating boys “reduces the pressure of having to vaccinate a large proportion of females”, Dr Gumel explained.
The study proposes immunising 65 per cent of the boys in the 12-17 population group while maintaining the current 80 per cent female vaccination coverage. Doing this will eliminate HPV-related cancers in South Korea within 60-70 years, the study estimates.
“The way to protect them is to surround them with a sea of immunity,” Dr Gumel said.
“We don’t have to be losing 350,000 people globally to cervical cancer each year. We can see an end to HPV and HPV-related cancers if we improve vaccination coverage.”