This post was originally published on here
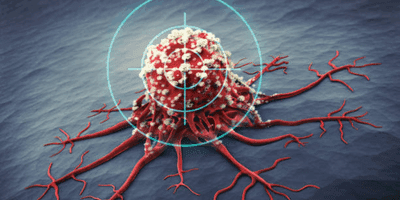
Cancer cells are basically the ultimate rule-breakers of the body. Under normal conditions, our cells follow a pretty strict set of instructions: grow when needed, stop when the job is done, and die when they’re old or damaged. Cancer cells, however, don’t get that memo or choose to ignore it completely. They keep dividing nonstop, piling up into lumps called tumors, or spreading silently through the blood and lymph system to other parts of the body.What makes cancer especially tricky is how sneaky it is. Even worse, cancer cells are great at hiding from the immune system, which is supposed to hunt down and destroy abnormal cells before they become a problem.Medical science has been fighting back hard. For decades, treatments like surgery, chemotherapy, and radiation have been the frontline defense cutting tumors out. While effective, these approaches can also harm healthy cells, which is why side effects happen. Today, things are getting smarter. Recently, scientists at KAIST have found a way to convert immune cells inside tumors into anticancer fighters.A research team led by Professor Ji-Ho Park of the Department of Bio and Brain Engineering has developed a therapy in which, when a drug is injected directly into a tumor, macrophages already present in the body absorb it, produce CAR (a cancer-recognizing device) proteins on their own, and are converted into anticancer immune cells known as “CAR-macrophages.”, KAIST has said. This will be useful for tumors found in gastric, lung, and liver cancers in which immune cells find it difficult to infiltrate the dense and solid tumors.
What are CAR-macrophages?
These are exciting new ideas in cancer treatment, and while they sound complicated, the basic concept is pretty simple. Macrophages are immune cells whose main job is to patrol the body, find threats, and “eat” things that don’t belong like bacteria, debris, or damaged cells.What makes CAR-macrophages especially interesting is how well they work inside solid tumors. Many immune cells struggle to enter the dense, protective environment around tumors, but macrophages naturally go there. Even better, CAR-macrophages don’t just attack cancer cells directly. They also send signals that wake up other immune cells, turning a quiet tumor into a loud immune battleground.This approach is still being tested in clinical trials, but early results are promising. Researchers hope CAR-macrophages could overcome some limits of existing treatments especially for solid cancers. While there’s more to learn, CAR-macrophages represent a smart, powerful way of re-teaching the immune system how to fight cancer.
Why does it matter?
Cancer isn’t rare. In fact, it’s one of the top causes of death around the world. Every year, millions of people hear those words, and the numbers keep going up as populations age and lifestyles change. The World Health Organization reports that nearly 10 million people died from cancer in 2020, that’s about one in six deaths. Treatments are getting smarter these days, many therapies are designed to hit cancer where it hurts, whether that’s a specific genetic mutation, a protein on the tumor’s surface, or some other weakness only cancer has. Targeted therapies like these can mean fewer nasty side effects, better results, and sometimes even faster recovery.Targeted therapies aren’t just about surviving, they’re about living better while you fight this relentless disease. That’s why patients, doctors, and researchers are so hopeful. These treatments offer more than just extra time; they offer a chance to keep your life as normal as possible while taking on cancer.