This post was originally published on here
“Hearst Magazines and Yahoo may earn commission or revenue on some items through these links.”
-
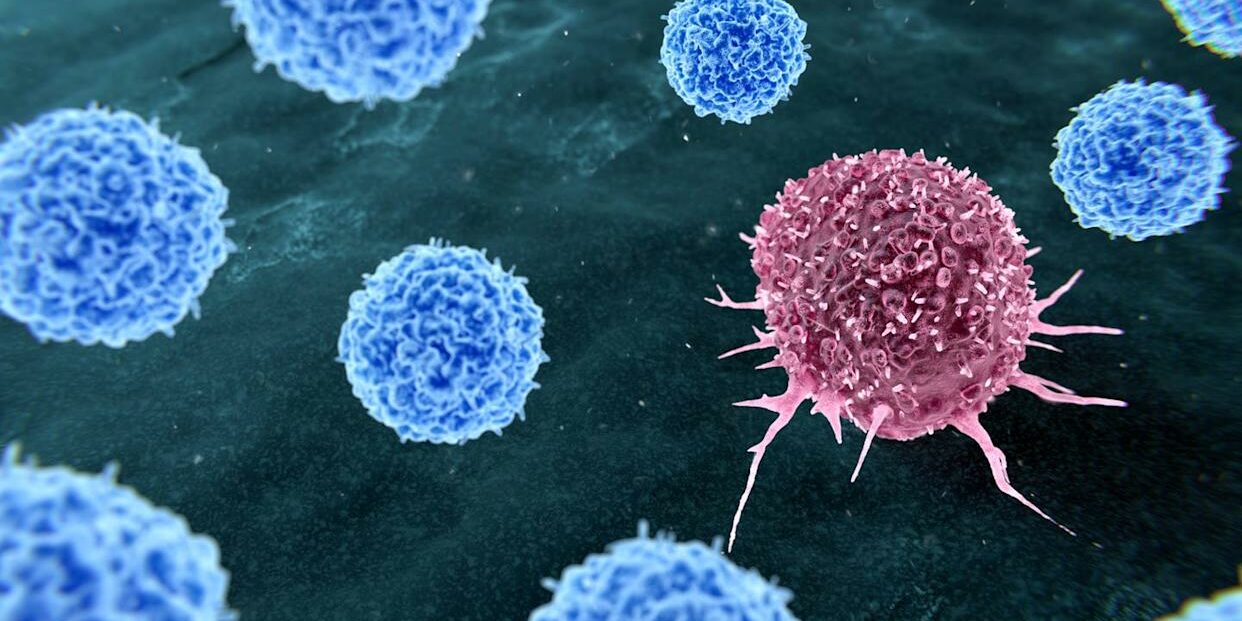
Scientists find that up to four in 10 cancer cases worldwide may be preventable.
-
In a recent study, researchers identified 30 preventable cancer causes, with tobacco, infections, and alcohol being among the biggest culprits.
-
An oncologist explains what the findings mean for you.
Cancer remains one of the leading causes of death worldwide, and rates of the disease are continuing to increase in people under 50, which may leave you wondering what you can do to reduce your risk. It turns out that making a few lifestyle tweaks could be a large part of the answer. New research suggests that up to four in 10 cancer cases worldwide may be prevented by adjusting eight specific lifestyle factors.
Meet the expert: Amar Rewari, M.D., chief of radiation oncology for Luminis Health and host of the Value Health Voices Podcast
After examining 30 causes of cancer deemed preventable as they may be avoided through behavioral changes, the study, published in Nature Medicine, estimated that 37% of 18.7 million new cancer cases in 2022 were attributed to preventable risk factors. The exact breakdown of cancer causes varied significantly by sex. Around 30% of cancer cases in women and 45% in men were deemed preventable.
Ahead, an oncologist breaks down the findings and what they mean for you.
What are the leading preventable causes of cancer?
The researchers identified several behavioral, environmental, and occupational cancer risk factors. The most prevalent causes, according to the study, include:
-
Tobacco smoking
-
Alcohol consumption
-
Obesity
-
Insufficient physical activity
-
Smokeless tobacco use
-
Air pollution
-
Ultraviolet radiation
-
Infection
The causes that appeared most often differed by region. “In higher-income countries, lifestyle factors like smoking, obesity, and alcohol play a larger role, while in lower-resource settings, infection-related cancers remain a major driver,” explains Amar Rewari, M.D., chief of radiation oncology for Luminis Health and host of the Value Health Voices Podcast.
The study outlines how cancer-causing infections may arise in lower-resource countries as early-life chronic infections that go untreated, brought on by overcrowding, poor sanitation practices, and lack of access to clean water, or as a result of low vaccine availability. Stomach cancer diagnoses associated with H. Pylori, a stomach infection, were particularly prevalent in areas of Japan and Korea, for example, while liver cancer diagnoses associated with hepatitis B and C infections were heavily represented in Africa. In both cases, increased access to vaccines and screenings has already led to a reduction in prevalence, though there’s still a long way to go.“This highlights the need for prevention strategies that are tailored to where people live and the risks they face, rather than a one-size-fits-all approach,” Dr. Rewari says.
Why are the findings significant?
The study’s findings may change the way we think about cancer prevention for the better by debunking common myths about cancer, according to Dr. Rewari. “They reinforce a powerful and often underappreciated message that a large share of cancer risk is not inevitable. Nearly 40% of cancers globally are linked to factors we already understand and, at least in theory, can change. This shifts the conversation from cancer being driven mainly by genetics or bad luck to one where prevention plays a central role,” he explains.
“One major takeaway is how consistently a small number of risk factors drive a large share of the global cancer burden,” Dr. Rewari points out. “Tobacco remains the single largest contributor worldwide, followed by infections such as HPV, H. Pylori, and hepatitis viruses, and then alcohol, obesity, and physical inactivity.”
The results also illuminate how cancer prevention has progressed over time. “Many of the biggest gains against cancer over the past several decades have come from reducing exposures, such as tobacco use and certain infections, rather than from treatment alone.”
What does this mean for you?
The good news is that simple behavioral and lifestyle changes play a consequential role in mitigating your risk of developing cancer. “Everyday choices and environments matter,” Dr. Rewari says. “Avoiding tobacco in all forms remains the single most important step to reduce cancer risk. Limiting alcohol, staying physically active, and maintaining a healthy weight can also make a meaningful difference over time.”
He also stresses the importance of staying up to date on your immunizations, such as the hepatitis B and HPV vaccines, “which are powerful cancer-prevention tools, not just infection-prevention tools.”
Still, while these actions may help reduce your chances of getting cancer, nothing you can do fully eliminates it. “Individual actions are important, but so are broader policies that support clean air, safer workplaces, and access to preventative care,” Dr. Rewari says. “Cancer prevention works best when people are supported by healthier environments and policies, not left to do it all on their own.”
The bottom line
The study’s findings seem promising, but more research is needed. “These numbers are based on large-population studies, so they’re meant to show big-picture patterns rather than explain why any one individual developed cancer,” Dr. Rewari says.
He also warns against reading too much into the term “preventable,” which “doesn’t mean that avoiding a single habit guarantees someone won’t get cancer. Many cancers develop over decades, and risk factors often overlap,” he explains. “Still, even with those nuances, the takeaway is clear, which is that reducing well-known risk factors at a population level could prevent millions of cancers over time.”
You Might Also Like