This post was originally published on here
Scientists have warned that a drug-resistant strain of a common fungus poses a serious threat to vulnerable patients in healthcare settings
A team of scientists has sounded the alarm over a drug-resistant strain of a common fungus, branding it a ‘global health threat’.
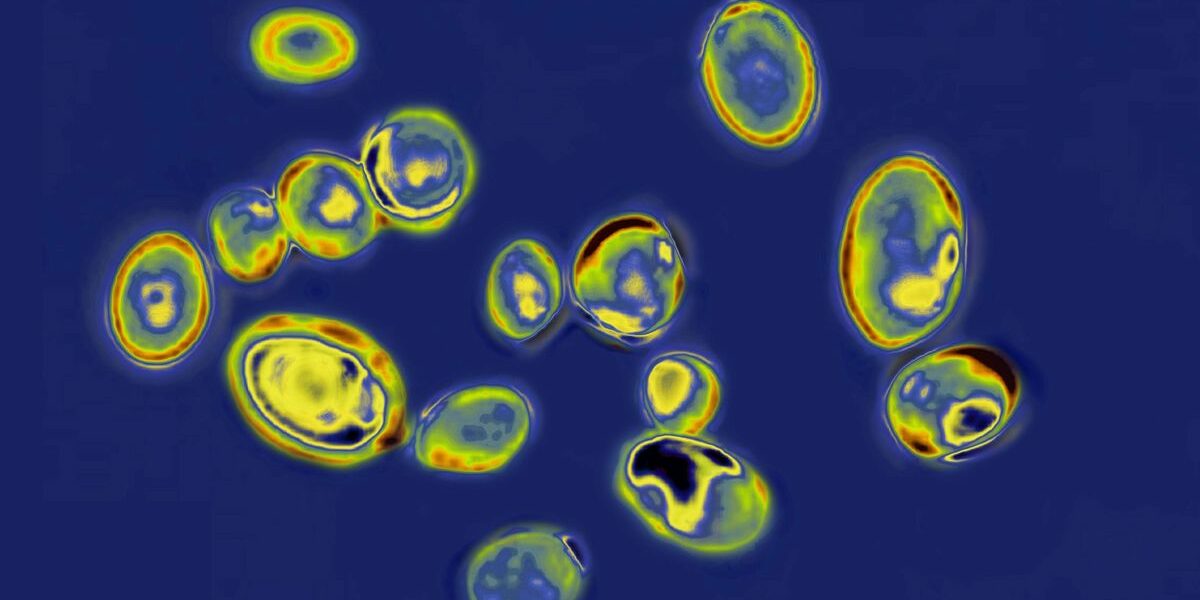
Candida auris (C. Auris), a type of yeast, can cause severe illness and is easily transmitted among critically ill patients in healthcare settings. The fungus can trigger anything from mild skin infections to more serious, potentially fatal conditions such as bloodstream infections.
Worryingly, it often develops resistance to antifungal medications, meaning it can outsmart the drugs designed to eradicate it. This resistance can render medical treatments ineffective. Each year, nearly 6.5 million people worldwide are affected by fungal infections. The difficulty in treating these infections can lead to a mortality rate exceeding 50%.
C. Auris poses a particular risk to individuals with compromised immune systems, reports the Daily Star.
First identified in 2009 in a Japanese patient’s ear canal, it has since been found globally and was declared a public health threat in India in 2014. C.
Auris can infect various parts of the body, including the blood, wounds, and ears. Symptoms depend on the location and severity of the infection.
They may resemble those of bacterial infections, such as fever or chills, but there isn’t a standard set of symptoms specific to C. auris infections.
“Candida auris (Candidozyma auris) is an emerging human fungal pathogen causing disseminated infections of high mortality (30–72%) in individuals with underlying diseases or impaired immunity,” the study reads.
“The pronounced skin tropism and pan-antifungal resistance of Candida auris pose a serious global health threat. A key question in C. auris biology is how clinical isolates acquire amphotericin B resistance.”
People can carry C. auris on their skin and other parts of their body whilst showing no signs of illness.
Healthcare experts term this state ‘colonisation. ‘ Those who are colonised can spread C. auris to nearby surfaces and items, as well as to fellow patients.
The investigation reveals that this fungus is rapidly evolving drug resistance by switching from a yeast-like form to a thread-like spreading system. Furthermore, it contains cell wall proteins enabling it to stick to human skin “like glue” and form settlements.
This microorganism is armed with “efflux pumps” on its cell membrane that can eject antifungal treatments before they can eliminate it. It also groups together to form adhesive biofilm coatings on surfaces, making it difficult for therapies to work effectively.
Rohini Manuel, consultant medical microbiologist at UKHSA, clarified: “C. auris rarely causes infections in healthy people although it can pose a risk to people in healthcare settings with weakened immune systems. Rates of C. auris in hospitals in England are very low, however they have been rising in recent years.
“UKHSA is working with the NHS to investigate the reasons behind this. Factors may include a rise in the fungus globally. Hospital outbreaks in this country are rare but we are supporting a small number of Trusts to limit the spread of C. auris.”