Scientist gives himself brain damage while testing secret experimental weapon
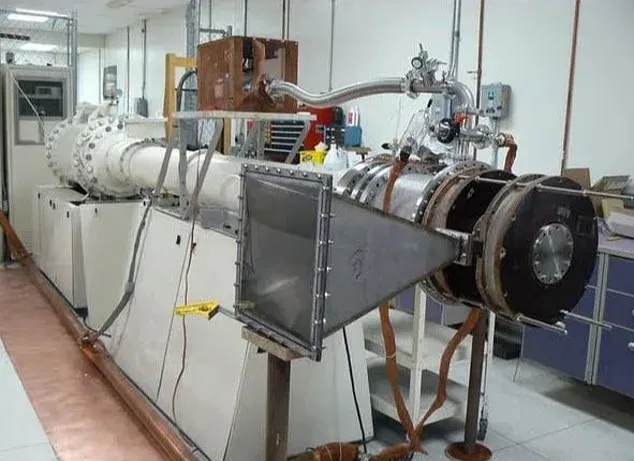
A Norwegian scientist has reportedly suffered brain injury … to as “Havana Syndrome.”
The scientist is said to have informed … have reportedly cautioned that the scientist’s symptoms do not exactly …